Whether it is the closure of a surgical incision or that of a laceration repair, a well-aligned wound approximation is the hallmark of a plastic surgeon. The best scar outcomes can only come from a beautifully closed wound. While good wound closure is not always a guarantee of a great scar result, poorly repaired tissue edges are a certainty to have a poor scar afterwards.
While these skin repair techniques provide excellent skin edge approximation and avoids undesired suture track marks, it does leave a fair amount of suture material at the most superficial layer of the tissues. While most of the suture material used for these closure techniques is resorbable, this does not mean that they always go away without causing some disturbing complications.
One of the most vexing wound problems from the incision line after surgery is the extruding suture/abscess. It is confusing for patients because of when it develops. Often not occurring for weeks to months after surgery, patients assume that they have an infection or a deeper wound problem. Patients understandably assume that wound healing is linear, meaning each day the wound appearance should continue to get better, but it isn’t. When an apparent well healed incision line develops an opening, drainage or a spot abscess weeks after surgery, patients are confused as to why it has occurred.
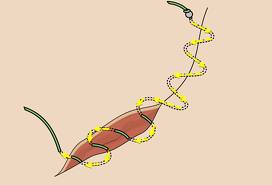
If the sutures were deep in the tissues this bodily reaction would never pose a problem. But in the skin, a small pocket of fluid around the knotted suture develops (which may progress to a small abscess like a pimple or pyogenic granuloma) and it begins to show through the suture line. A ‘hot spot’ will develop which will usually erupt through the skin and drain. Because the resorption time of all sutures used for these wound closure methods takes often six months or longer, the body’s inflammatory response occurs far quicker than the suture’s ability to resorb. When these suture extrusions involve a subcuticular stitch, it can act as a wick spreading the infection a great distance along the wound closure line.
Treatment of extruding sutures and their abscesses ultimately requires that the suture be removed, or the problem will continue to fester. In some cases, the suture extrudes innocuously many months later without any inflammatory reaction. This can be harder to appreciate because many of these suture materials are colorless and the only sign is a small opening along the incision line.
The most likely problems with extruding sutures is on long incisions from body contouring procedures. Tummy tucks, breast reductions, thigh lifts and arm lifts, all which involve extensive wound closures, are the most common procedures where these types of suture reactions are most likely to be seen. Why some patients get none, experience just a few and others have large number of extruding sutures in these wound closures is not clear.
Dr. Barry Eppley
Indianapolis, Indiana


