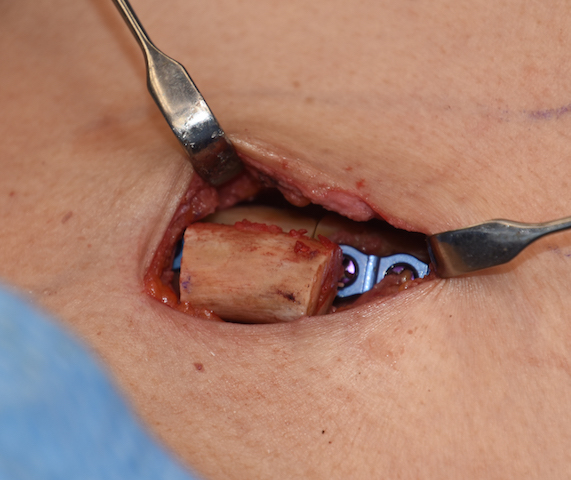
Shoulder reduction surgery is done to create a more feminine appearance whether it is in the transgender male to female or the cis-female patient. It is done by removing a segment of bone from the clavicle which subsequently brings the shoulders more inward. (decreased bideltoid distance)
One of the key aesthetic questions about this operation is how much shoulder width reduction is achieved relative to the amount of bone removed. It is assumed that it is essentially a 1:1 ratio although no formal studies have ever yet been done on this procedure due to the current low number of patients who have had the surgery. The visible reduction in shoulder width is a function of both reductions in horizontal clavicle length as well as some anterior forward rotation of the shoulders. The rounding effect of the shoulders comes from the anterior rotation which appears to be relatively minor as it relates to perceived width reduction.

To answer these important questions one has to go to the orthopedic surgery literature and look at clavicle fractures…which is not necessarily a direct corollary to elective clavicle reduction. Most clavicle fractures are mid shaft and often spiral in contrast to clavicle osteotomes which are in the medial third and create a direct healthy end to end bony alignment without minimal surrounding soft tissue trauma.
But the common nature of clavicle fractures and loss of bone length has been studied in relation to functional shoulder motion. (specifically acromioclavicular and glenohumeral joint function) Since the clavicle acts as the only strut between the thorax and the scapula and upper arm, it is reasonable to presume that loss of length may adversely affect shoulder function and is the primary motivation for open reduction and internal fixation of clavicle fractures. Non-operative clavicle fracture healing typically shows clavicle shortening due to superior displacement of the medial bone segment. This purportedly results in a change in the resting position of the scapula. (protraction and downward rotation) This could potentially lead to post injury abnormal scapular movements during functional activities. (loss of strength, possible subacromial impingement)
But in the most recent comprehensive study that I have read which investigated scapular orientations and functional outcome in healed clavicular fractures with resultant bone shortening, no relevant adverse functional outcomes occurred. In this study the mean clavicular shortening was 25 mm. Scapula protraction had increased very slightly in rest position in the affected shoulder. During abduction, there was slightly more protraction and slightly less backward tilt in the affected shoulder. For anteflexion, the scapular orientations of the affected shoulders also showed slightly increased protraction, slightly increased lateral rotation, and slightly reduced backward tilt. Bit none of these modest scapular positional changes had any loss of muscular strength or range of motion.
The corollary from the orthopedic literature and the assessment of scapulohumeral kinematics in mid shaft clavicle fractures with bone shortening indicates no negative shoulder functions should occur in elective clavicle length reduction. That has certainly proven to be true in the shoulder width reduction surgeries I have done. It indicates that the range of 2 to 3cms loss of clavicle length is safe. Shortening beyond 3 cms , however, has unknown sequelae for shoulder function and should be considered accordingly. Such a larger amount of bone length removal is a theoretical one since patients seem to be very pleased with their shoulder appearance after lesser amounts of clavicle bone length loss.
Dr. Barry Eppley
Indianapolis, Indiana