The treatment of tear trough and related nasojugal grooves has evolved over the years to include injectable fillers, fat and infraorbital implants. Each method has their advantages and disadvantages and none of the available treatments are perfect or free of complications. Patients with tear trough deformities can be young or older with the difference in the older patient that they may need an open blepharoplasty due to other eyelid aging issues. The younger patient usually just has tear trough or infraorbital hollow deficiencies without loose lower eyelid skin or muscle or fat prolapse.
For purposes of anatomic clarification, one should understand the differences between the two common infraorbital deformities of the tear trough and nasojugal grooves. A tear trough is a deep groove that commonly occurs beneath the lower lid, near the junction of the eyelid and cheek skin, beginning near the inner canthus and descends obliquely and laterally down the cheek for one or two centimeters. This is to be differentiated from the nasojugal groove which is caused by a natural muscular defect that occurs between the orbicularis muscle and the angular head of the elevator superior labii muscle combined with orbicularis-orbital septal adhesion to the bony orbital rim.
The problem with both injectable fillers and fat is the lack of placement precision, risk of visible lumpiness and lack of permanency. Infraorbital implants address all of these concerns fairly well but have an underutilized role in the treatment of these suborbital defects because it is an invasive procedure. There is also a lack of anatomic knowledge and good technique amongst surgeons in their placement which also leads to a perception that they have a ‘high complication rate’.
For patients undergoing lower blepharoplasty for aging concerns good improvement of tear troughs and nasojugal grooves can occur with release of the lower lid orbicularis muscle attachment to the infraorbital orbital rim combined with cheeklifting and lateral canthopexy anchoring. However, in young patients and in the older blepharoplasty patient an implant adds both volume and serves as as spacer between the muscle and bony rim which provides an assured volume addition effect.
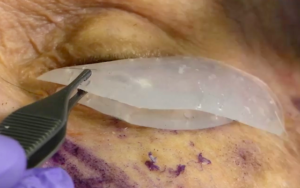


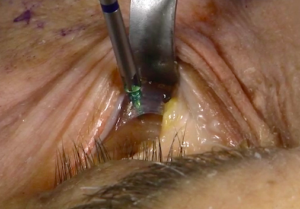


Infraorbital or suborbital implants are effective for tear trough and nasojugal reduction/eradication. They can be placed either through a transcutaneous or transconjunctival approach. In younger patients with no significant periorbital aging transconjunctival implant placement may be adequate. In older patients a lower eyelid skin-muscle flap approach to implant placement with cheeklifting and lateral canthopexies is a powerful lower blepharoplasty combination. The extended infraorbital implant can also help with malar hypoplasia that often involves the infraorbital rim as well.
It is important to appreciate that these standard suborbital implants augment the anterior surface of the bone and produce horizontal augmentation. They will not be effective for infraorbital hollowing with lid sag and increased scleral show which represents more of a vertical infraorbiral rim deficiency. This is better addressed through custom infraorbital or infraorbial-malar implants.
Dr. Barry Eppley
Indianapolis, Indiana








