Functional nasal airway surgery is intended to improve breathing though your nose by removing mechanical obstructions to airflow. Many patients confuse this type of nasal surgery with rhinoplasty which is the external reshaping of the nose. (particularly as it relates to insurance coverage!) This is understandable given that it is quite common to do both at the same time, simultaneously improving most of the major functions of the nose in a one surgery.
Nasal airway surgery almost always involves efforts to straighten the septum. While this central piece of cartilage (and bone in the back) separates the two sides of the nose, it is frequently not straight. As a result, septal straightening or septoplasty, is synonymous with better breathing as it may be deviated to one side which reduces airflow in at least half of the nose.
Inferior turbinate reduction is done as commonly as septoplasty for airway improvement. There have been many methods to reduce the size of the turbinate. Most of these involve cutting or cauterizing it. While these are effective, they are also prone to cause bleeding during and after surgery and are a common source of postoperative bleeding. A recent article in the June 2009 Plastic and Reconstructive Surgery journal looked at another method that is less invasive for turbinate reduction…that of outfracturing.
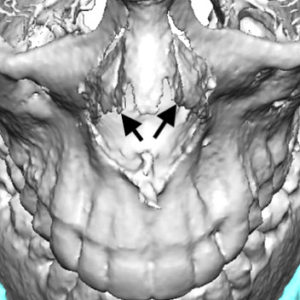
Outfracturing of the inferior turbinate is the simple procedure of breaking the thin bone contained within it and moving it to the side. By so doing, the airway is opened as the turbinate is made ‘smaller’. The combination of septal straightening and turbinate relocation can really open up the nasal airway. The authors of this journal article looked at, with CT scans, whether inferior turbinate reduction by outfracturing resulted in a sustainable long-term improvement in the nasal airway. Their results shows that it provided a measureable improvement (around 25%) that was indeed maintained and did so without any complications such as bleeding.
Inferior turbinate reduction is an integral part of functional nasal airway surgery. In my Indianapolis plastic surgery practice, I have used outfracturing for some time and have been impressed that it appears to be effective despite its simplicity. This study reported in this June article provides scientific evidence to continue with this turbinate management method.
Dr. Barry Eppley
Indianapolis, Indiana


