brow bone reduction, technical strategies
Technical Strategies – Transpalpebral Tail of the Brow Bone Reduction
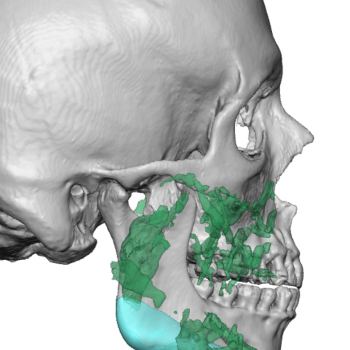
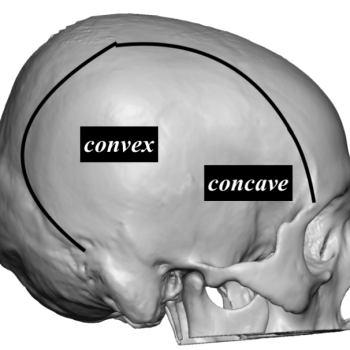
Brow bone reduction is a recognized facial reshaping procedure to reduce the prominence of the lower forehead. In doing so the reduction is in a reverse horizontal...
Top Articles
-
Clinical Outcomes in Rib Removal Surgery for Waistline Reduction
Rib removal surgery represents the elimination of the last anatomic...
-
The Surgical Technique of Clavicular Osteotomies in Shoulder Width Reduction
Shoulder width reduction is done by shortening the length of the...
-
Masculinizing the Male Forehead with Custom Brow Bone Implants
The shape and appearance of the forehead is highly influenced by...
-
Case Study: Lengthening of the Nose with a Rib Graft Rhinoplasty
Background: The evolution of rhinoplasty surgery over the past twenty years...
-
custom facial implants, injectable fillers
Injectable Fillers and Custom Facial Implant Designs -
chin implants, plastic surgery case study, sliding genioplasty
Secondary Chin Implant Augmentation After Sliding Geniopalsty – A Case Study -
plastic surgery case study, temporal reduction
Understanding Temporal Reduction Surgery: Anatomy, Technique, and a Case Study
Dr. Barry Eppley
Dr. Barry Eppley is an extensively trained plastic and cosmetic surgeon with more than 25 years experience. He is both a licensed physician and dentist as well as double board-certified in both Plastic and Reconstructive Surgery and Oral and Maxillofacial Surgery. This training allows him to perform the most complex surgical procedures from cosmetic changes to the face and body to craniofacial surgery. Dr. Eppley has made extensive contributions to plastic surgery starting with the development of several advanced surgical techniques. He is a revered author, lecturer and educator in the field of plastic and cosmetic surgery.