Background: The chin is the prominent and most protruding structure of the lower face. It is a three-dimensional facial part that can have excesses and deficiencies of either the amount of projection, width or in its height. Because of the soft tissue that wraps around the chin bone, excessive or big chins pose greater aesthetic challenges than that of the small chin.
Having a big chin can involve any (or all) of the three dimensions and the surgical technique to reduce it varies based on these dimensions. In order of difficulty, the wide chin is the simplest to effectively change and the horizontal overprojecting chin can be the most challenging. The vertically long chin offers an intermediate level of difficulty, and like the chin that sticks out too far, the biggest challenge is how to predictably shrink the enveloping soft tissue to avoid a postoperative sag.
The vertically long chin can be reduced by two methods. The traditional approach is to use an intraoral osteotomy (genioplasty) and remove a wedge of bone either from above or below the osteotomy cut. The main advantage of this technique, besides the avoidance of an external scar, is that the soft tissue attachments to the underside of the chin bone are not disrupted. The alternative approach is to remove the bone from below through a submental incision, detaching and then reattaching the neck and chin soft tissues after the bone is removed. The advantage of this approach is that any redundant soft tissues of the chin can be directly removed and tightened and the superior attachments of the mentalis muscle is not disrupted.
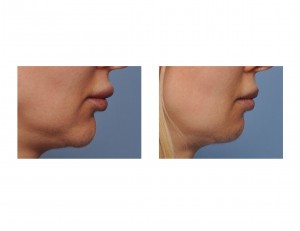
Case Study: This 40 year-old female wanted a shorter and less long chin. She had a chin implant placed at the time of a previous rhinoplasty, at the suggestion of her surgeon, but it made her chin too big and it was subsequently removed. Despite its removal, she still wanted an even shorter chin. She acknowledged that she already had a small chin, by everyone else’s standards, but to her it was still too big. She just wanted the bottom part of it ‘cut off’.


Case Highlights:
1) The length of the chin can be successfully reduced like other chin dimensions.
2) Vertical reduction of the chin can be done through either an intraoral wedge ostectomy/genioplasty or a submental ostectomy, of which the intraoral approach is the most common.
3) The submental vertical chin reduction removed the lower end of the chin bone as well as excises and resuspends the soft tissue chin pad and upper neck tissues.
Dr. Barry Eppley
Indianapolis, Indiana


