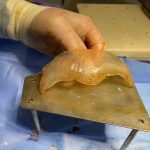
OR Snapshots – How To and Not To Perform a Feminizing Rhinoplasty

Rhinoplasty surgery has tremendous capabilities of changing the shape of the nose. In doing so there are many tried and true techniques of how to do it successfully as well as how to maintain the result long term. Despite the many techniques available to change the structural framework of the nose, there are no established Read More…