The development of retraction or lid sag is the risk that every open procedure done on the lower eyelid risks. Despite known efforts to prevent it, such as lateral cantopexies, limited skin resection and orbicularis muscle resuspension, it can still develop in some patients. Many mild cases that occur right after surgery in a patient with good lateral cantonal tendon support (good preoperative snap test) will gone ton o resolution with time and conservative management strategies. (taping and massage)

In the March 2019 issue of the journal Plastic and Reconstructive Surgery, an article was published entitled ‘Correction of Lower Eyelid Retraction with EnGlove Placement of Porcine Dermal Collagen Matrix’. In this paper the authors describe their ‘minimally invasive’ technique for the correction of mild to moderate lower eyelid retraction. An initial canthotomy is performed with inferior cantholysis followed by blunt dissection in the subconjunctival plane. A subconjunctival pocket is made across the inside the lower lid through which a porcine collagen sheet is placed. Placement is along the inferior edge of the tarsus. The graft is secured into placed with through and through sutures. Closure is then done with a lateral tarsal strip procedure. A lateral lower eyelid suspension suture is than applied to the forehead.
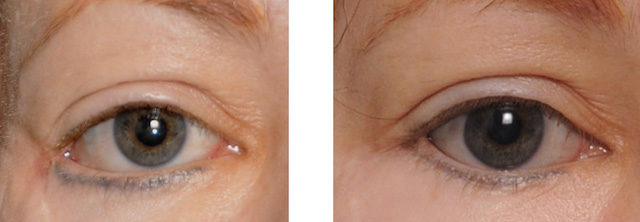
A total of nine patients (ten eyelids) with an average of 72 years old. With a mean followup of nine months all patients showed correction of the retraction and iimprovement n the shape of the lateral canthal angle. Two complications occurred which required treatment, one of graft placement and the other with recurrent lateral canthal dystopia.
The crux of this technique is that is is done with a tunnel approach to pocket placement of the spacer graft. I don’t think the type of allogeneic collage matrix matters in any way and other types of such collagen sheeting can be used. Patient selection is key as a minimally invasive technique logically will work for those with similarly matched preoperative problems. The authors use the criteria of 3mms or less of retraction, adequate lower eyelid skin and lack of a negative orbital vector.
This technique, while not applicable to all cases of ectropion, has a useful role to play in milder refractory cases and avoids a lower blepharoplasty incision. Getting the graft in the right place and laying flat is the key element in the technique since it is done in a more blinded fashion.
Dr. Barry Eppley
Indianapolis, Indiana