
In the October 2014 issue of the journal Plastic and Reconstructive Surgery, an article appeared entitled ‘Facial Feminization Surgery: The Forehead. Surgical Technique and Analysis of Results’. Over a four year period, the authors performed 172 forehead reshaping procedures. The results were assessed by cephalometric x-rays and a six month after surgery survey. The specific techniques discussed were incisional access and how the bone areas are specifically reshaped. Incisional access was done through either a hairline (pretrichial) or modified coronal based on the vertical length of the forehead and whether hairline lowering was simultaneously needed. The bone was reshaped through sequencing of frontonasal-orbital reconstruction/recontouring with osteotomy and setback of the anterior wall of the frontal sinus.
No serious complications were observed in this forehead feminization patient series. No hematomas, seromas or infections occurred. There were no complications related to osteotomizing the anterior wall of the frontal sinus such as sinus dysfunction, sinusitis, mucoceles, or air leaks. One patient did develop a cerebrospinal fluid leak from the posterior wall of the frontal sinus that resolved spontaneously within days after surgery by posture measures. Most patients had some degree of forehead numbness with complete recovery starting three months after surgery. No permanent injury to the frontal branch of the facial nerve occurred although some patients had some weakness which fully recovered weeks after surgery. The average level of patient satisfaction by the after surgery survey was between satisfied and completely satisfied.
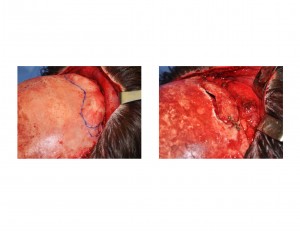
Despite the rather invasive nature of this type of forehead surgery, complications are remarkably few and significant improvement is always seen. There can be issues that may require secondary revision such as the smoothness of the brow region. This article does not address whether any revisions were required but some low percent can be expected. (3% to 5%)
Brow bone reshaping and associated hairline modifications can effectively alter masculine facial features in the transgender patient with a very low incidence of negative side effects. To really change the forehead/brow area a comprehensive bone and soft tissue approach is needed.
Dr. Barry Eppley
Indianapolis, Indiana


