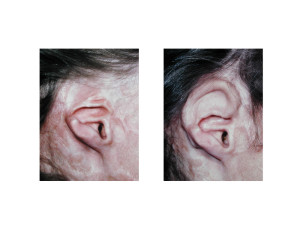
Ear reconstruction is challenging and is put to the test when portions of the ear are lost from a burn injury. Burned ears present with a unique situation due to the pattern of ear loss. Almost always the external auditory canal and the cartilaginous tragus and portions of the antihelix may remain. But the outer helix and earlobe are often lost due to the greater exposure of the outer framework of the ear to the heat source.
Maintenance of the external auditory canal and the surrounding cartilage is always beneficial in ear reconstruction as these ear areas can be the hardest structures to surgically recreate. But the burnt tissue around the remaining stump of the ear, which has usually been skin grafted, poses a dilemma for outer ear framework reconstruction. The skin is not pliable and can not be used/elevated to provide any skin coverage over a helical cartilage reconstruction.
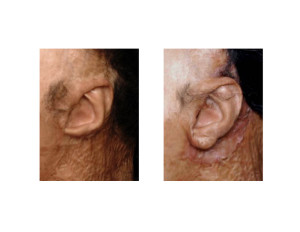
There is also a third approach where an ear cartilage framework is covered by a pedicled temporal fascial flap. This requires of course an intact temporal artery pedicle which may or may not be present. The fascial flap covers the framework and is then skin grafted.
The burn ear deformity presents a different reconstructive challenge than that of congenital microtia for example. It suffers from poor quality surrounding skin cover and thus requires a different strategy for providing soft tissue coverage over a cartilage framework reconstruction.
Dr. Barry Eppley
Indianapolis, Indiana


