Background: Hemifacial microsomia is a well known congenital facial deformity that affects the structures that develop from the first and second brachial arches. As a result anomalies develop that includes the ear, lower jaw and mouth areas. It is a spectrum of deformities which cause varying deformities of these facial structures and, while typically occurring just on one side, can also present on both sides. It is the second most common congenital facial deformity behind that of cleft lip and palate.
The treatment of the jaw deformity of hemifacial microsomia is mainly a bony one but often includes that of the soft tissue as well. The lower jaw fails to grow properly and is often treated by mandibular distraction in infancy or as child. But ultimately most patients need orthognathic surgery in late adolescence which may be just lower jaw advancement but more commonly requires bimaxillary surgery to realign both the upper and lower jaws.
With the underdeveloped lower jaw is that of an associated soft tissue deficiency as well. The thickness of the soft tissue over the jaw angle area is thinner and this is no surprise given that what lies between the ear and jaw is equally affected. Such soft tissue deficiency can be treated by fat injections, dermal-fat grafts and free tissue transfer depending on the magnitude of the deficiency. In most cases some form of fat transfer is usually done.
Case Study: This late teenage male had bilateral hemifacial microsomia with a vey short lower jaw, an anterior open bite and bilateral soft tissue deformities in front of the ear over the jaw angle areas. Even though he ideally needed orthodontics and bimaxillary orthognathic surgery, this was not an option he wanted to pursue. Thus the focus was on getting him more chin projection and additional soft tissue fullness over the lateral jaw angle facial areas.

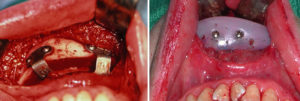

In a thin patient like this one, fat harvesting by liposuction would be inadequate and the injected fat survival in the tight hypoplastic soft tissues would probably not be very good. Dermal-fat grafts, while not commonly used today, still have a valuable role to play that produces a greater soft tissue fill/push and has a high survival rate.
Case Highlights:
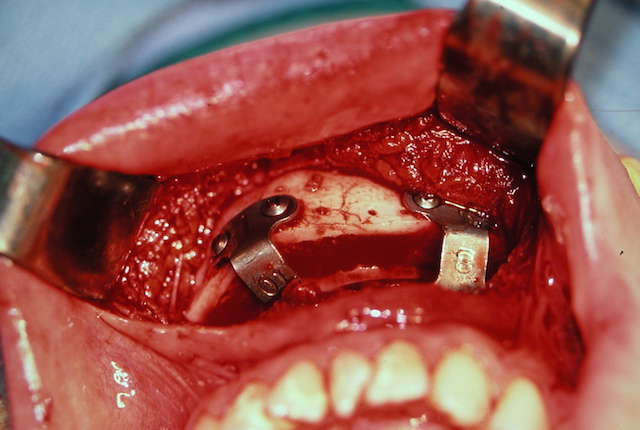
1) In large chin advancements a sliding genioplasty can be combined with a chin implant overlay for maximal projection.
2) When knowing a composite chin augmentation is needed, it is best to keep the sliding genioplasty at 10mms advancement to provide room for the implant.
3) Soft tissue deficiencies over the jaw angle areas in thin patients are best treated by use of large dermal-fat grafts in a thin patient.
Dr. Barry Eppley
Indianapolis, Indiana