Background: Cheek implants have been used for aesthetic facial augmentation for over fifty years. While the shape and numerous implant styles has changed over the years, the basic concepts of their placement remain the same. Through an intraoral approach a subperiosteal pocket is developed over the cheekbone where the implant is designed to sit. The main historic debate is how to secure the implant into the pocket as it really is ‘hanging off the edge of the bone’ since it is an implant placed on the side of the cheekbone. This usually creates cheek fullness which is often described as varying degrees of an apple cheek look. This may be a good aesthetic effect for some women but often not so much for men.
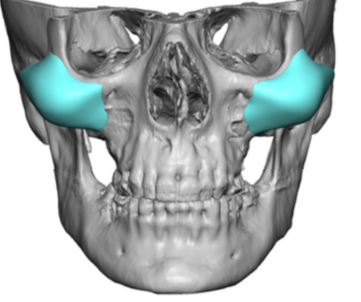
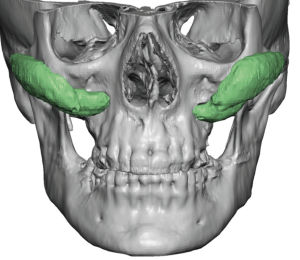
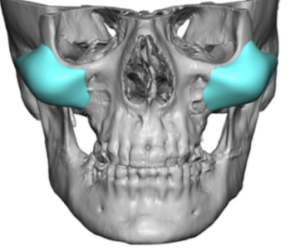
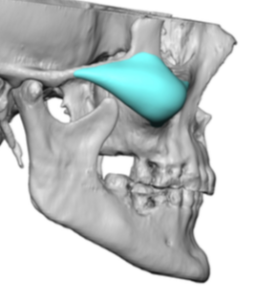
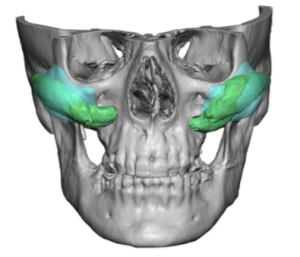
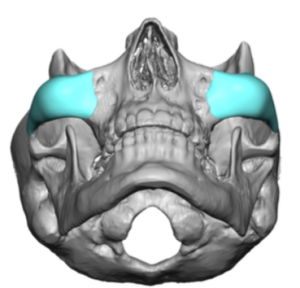
In contemporary cheek implant augmentation it has evolved into the potential for improved designs that can create different types of midface shapes. Most pertinently the high cheekbone look is what many patients seek today…almost all men do and many women do as well. This is not what most standard cheek implant styles can satisfactorily create. Standard cheek implants are oblong in shape and sit obliquely on the bone while the high cheekbone implant is more longitudinal in shape and sits more horizontally on the bone.
Existing cheek implant patients may appear from which their implants were placed decades ago. They are older now and what worked for them back then may not be as aesthetically effective today. In thin faced patients their cheek implants may appear unnatural as a distinct mass that has a separate shape from the bone. This is function of a lack of soft tissue thickness but equally occurs because the implant was designed and placed for a partial soft tissue effect and not a pure bony one. It may also be that the implants are not really visible but that the apple cheek look is now excessive as some soft tissue ptosis has occurred from aging.
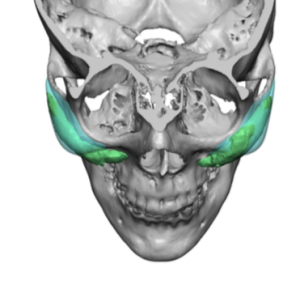

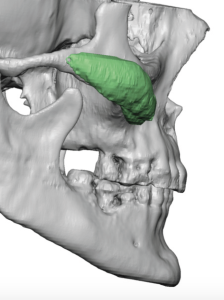
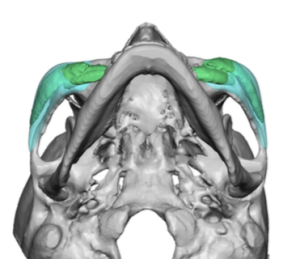
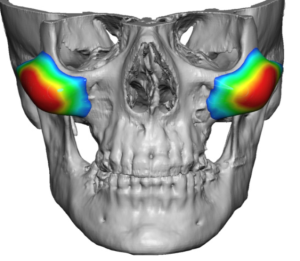
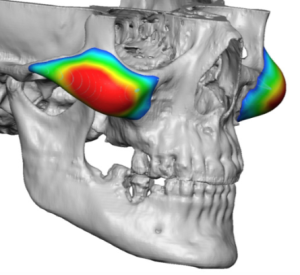
In custom facial implant designing the adage of ‘when you never what does not work well you know how to design it better’ always applies when indwelling implants exist. Being able to see them on a 3D CT scan provides an immense help for a new implant design improvement. One unique feature of. any custom facial implant design is that the line of augmentation can be determined by looking at the colorized thicknesses on the implant design.
Case Highlights:
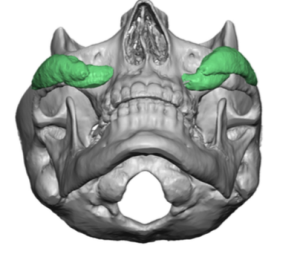
1) Replacing indwelling cheek implants with an improved shape requires a custom cheek implant design process where both implants are seen and overlaid.
2) Many cheek implants that have been in for a long time are associated with varying degrees of benign heterotypic calcifications.
3) Facial aging and the desire for high cheekbone look in females requires a design where most of the volume is away from the submalar space.
Dr. Barry Eppley
Indianapolis, Indiana