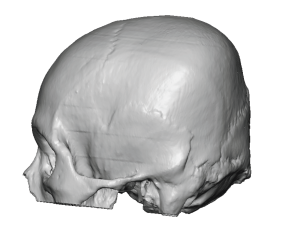
Background: While the most common non-synostotic congenital skull deformity is plagiocephaly, less commonly seen is its ‘cousin’ brachycephaly. As opposed to a unilateral flattening on the back of the head in plagiocephaly, brachycephaly is when the entire back of the head is flat. While it can have synostotic origins like some forms of plagiocephaly most brachycephalies new deformational in nature with prolonged laying on the back of the head as a baby as the most recognized cause.
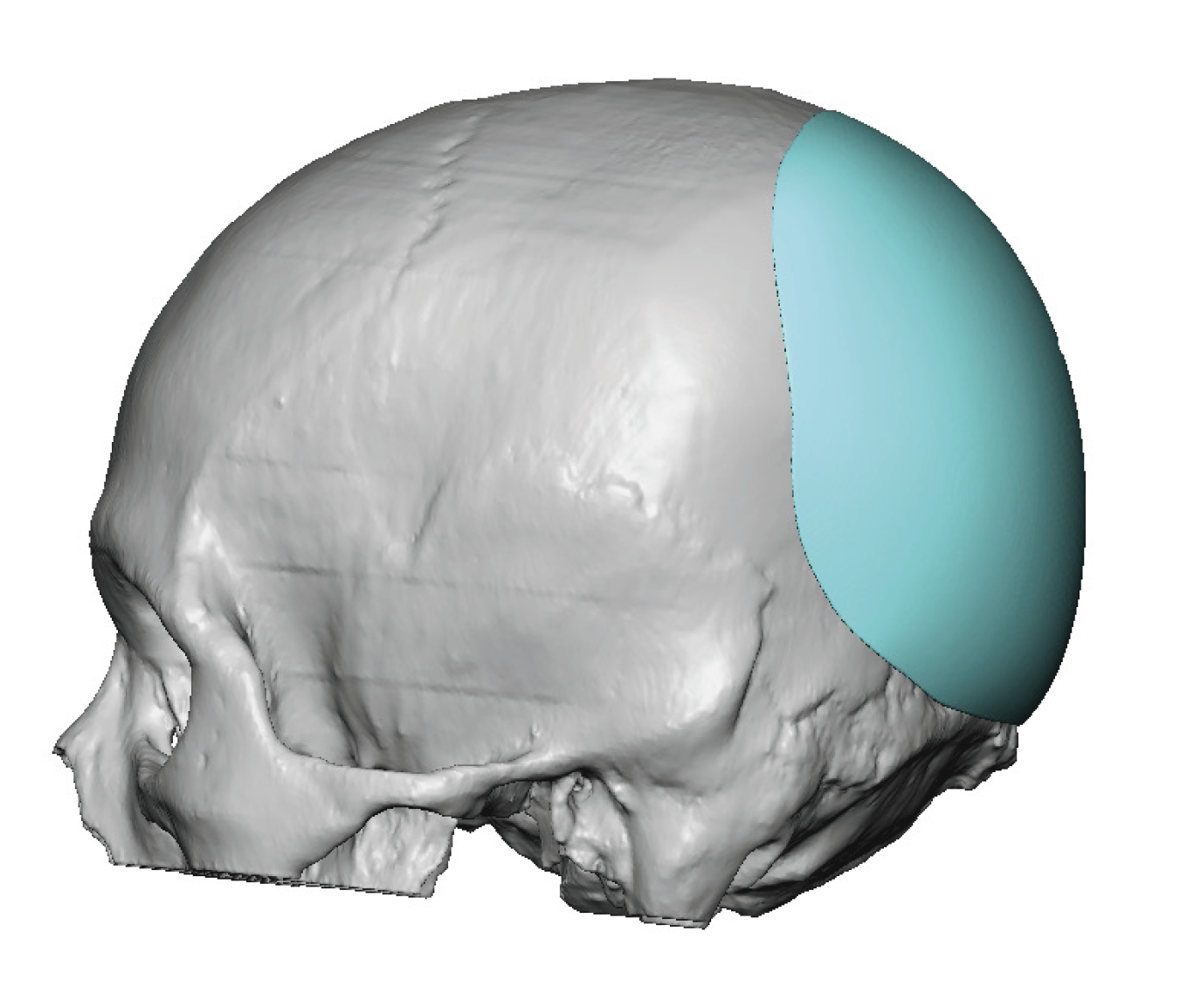
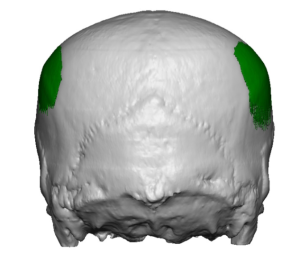
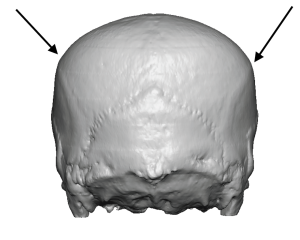
In adults with brchycephaly the need for increased projection of the back of the head is obvious. But a concomitant show issue is that the lack of projection has been compensated for with brain growth by having increased width. This width is most pronounced at the junction of the posterior temporal and parietal bones along the bony temporal line. Patients so affected know this well as they see their head being too wide at the sides in the front view. While the lack of posterior head projection is best seen in the side views patients are well aware of the entire back of the head problem with ill-fitting hats, helmets and work head gear.
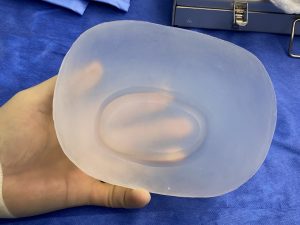
While brachycephaly may be treated by cranial vault remodeling in infants and very young children that is to an option in adults. Rather than treating the root cause of the problem (full thickness skull osteotomies/reshaping) an exterior camouflage a[[roach through outer surface skull reshaping techniques is needed.

Case Highlights:
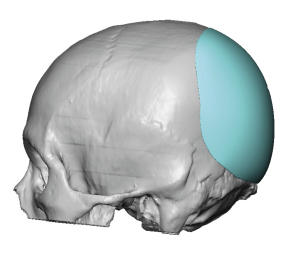
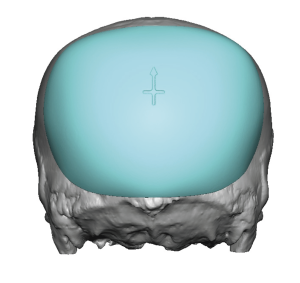
1) Flattening of the entire back of the head (brachycephaly) is often associated with bilateral temporo-parietal widening, particularly in the more severe cases.
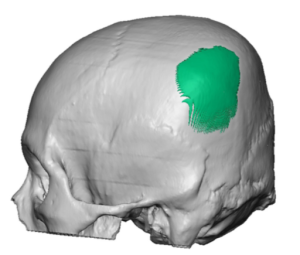
2) While added projection of the back of the head in brachycephaly is the most beneficial dimensional change with a custom skull implant design, reducing the projection of the ‘corners’ (temporo-parietal edges) also provides some additional shape benefit.
3) A triangulation small incisional pattern provides access to do complete reshaping of the back of the head.
Dr. Barry Eppley
World Renowned Plastic Surgeon