Background: The correction of congenital skull deformities with early cranial vault reconstruction is a well established surgical therapy. Such early skull manipulations are based on two fundamental principles of the infant’s skull. First, the bone is thin and can fairly easily be removed, reshaped and re-inserted. Secondly, the osteogenic regenerative power of the dura at such early ages allows any bone defects around the bone reconstruction to fill in with new bone.
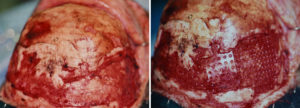
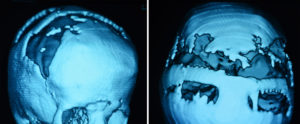
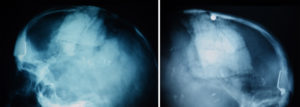
But despite the potential osteogenic capability of the dura in infants, full-thickness bone defects still do occur. Often they are small and are at the junction of reassembled skull bone pieces from the initial reconstruction. But in rare cases the skull defects may be much bigger, reflective of bone defects left behind from large bony advancements from contour expansions.
The reconstruction of skull defects in children can be done by a variety of methods. While bone may be considered an ideal material, the successful splitting of cranial bone in children is not an assured outcome. A variety of synthetic materials and implants are available to ‘patch’ such skull defects. Each has their own unique handling characteristics.
Highlights:
- Full thickness skull defects are not rare after infantile cranial vault reconstruction surgery.
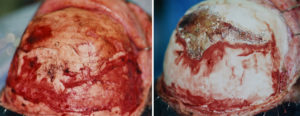
- While hydroxyapatite cement may be the best reconstructive material choice for the pediatric skull, its weak biomechanical properties are not favorable to be used alone.
- Creating a stable floor with resorbable mesh plates allows hydroxyapatite cement to be successfully applied in full thickness skull defects in children.
Dr. Barry Eppley
Indianapolis, Indiana