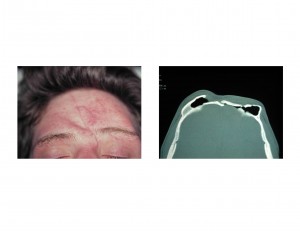
Background:The forehead occupies the upper third of the face and has variable degrees of convexity based on gender and genetics. It is structurally composed of very strong bicortical bone at its upper two-thirds and the much weaker aerated brow bones at its lower third underneath the eyebrows. While the forehead can resist significant forces, up to more than 100kgs of impact, it can be fractured and displaced. The brow bones, however, fracture at much lower impact forces.
Because it takes such a tremendous force to fracture the frontal bone, most such injuries also cause brain trauma and frequently need neurosurgical intervention. Often a craniotomy is done and the forehead bone is reconstructed at that time. But some cases do not involve the need for neurosurgery and the forehead defect is lefted untreated. These forehead contour defects are then reconstructed secondarily.
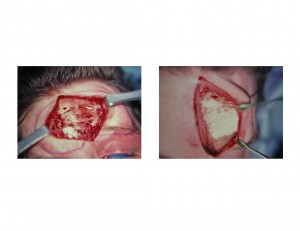

The hydroxyapatite cranioplasty concept is now about 15 years old in its clinical use. It offers an advantage over old-style PMMA (acrylic) in that the material is more biocompatible and actually integrates into the tissues. It is more expensive than PMMA and is far less impact/fracture resistant.But I have never yet seen that be a secondary cranioplasty problem. Due to the handling of the material it must be placed through an open approach. In some cases, small incisional access can be used to place the material.
Case Highlights:
1) Forehead defects from trauma involve changes in the contour of either the solid portion of the forehead and/or the more fragile brow bones.
2) Contour reconstruction of the depressed forehead can be done with the onlay cranioplasty material, hydroxyapatite, in an open technique.
3) Frontal cranioplasty can be done through either a coronal (scalp) incision or an existing forehead laceration if it is big enough.
Dr. Barry Eppley
Indianapolis, Indiana


