Background: Occipital plagiocephaly is a well known benign skull deformity that causes a rather classic flat spot on the back of the head. It is frequently present at birth due to the positioning of the neonate head in the womb. It can also be caused by positioning of the baby during sleep causing a constant pressure force on one side of the back of the head. Regardless of the cause, occipital plagiocephaly can be improved by positioning techniques early after birth or molding helmet therapy in the first year of life.
But once occipital plagiocephaly persists beyond one year of age, there are no external methods that can create a significant correction. Cranial vault remodeling can be done but the extent of this surgery makes it only justified in the most severe cases. Otherwise, flat spots on the back of the head must be endured to perhaps be dealt with as an adult if its appearance is a concern.
Skull augmentations in adults are not infrequently done for a variety of shape issues from the forehead to the back of the head by onlay cranioplasty methods. Through scalp incisions of various lengths and locations, different bone cement materials can be applied and shaped to change the skull contours in the treated area. Most commonly, the bone cement material is PMMA (acrylic) due to its lower cost and easy shaping in tight spaces.
Case Study: This 4 year-old male child had a moderately flat right occiput. On examination it could be seen that he had many of the typical findings for occipital plagiocephaly with some contralateral skull flaring/widening and a more forward position on the flattened. The parents were concerned with his degree of skull deformity and wanted to see it improved before he was much older and potentially subject to peer criticism.

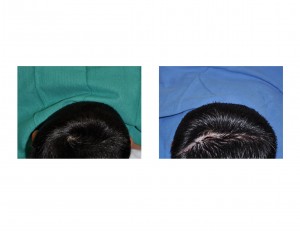
While the decision to undergo skull reshaping in children for a flat back of the head can be viewed as controversial by some, that is a personal decision for parents to make about the need for surgical improvement in their child. From a plastic surgery standpoint, the onlay cranioplasty procedure is safe and effective and has few drawbacks other than a fine line scar in the scalp to perform it.
Case Highlights:
1) Occipital plagiocephaly can be treated at any age by an onlay cranioplasty skull reshaping technique.
2) The cranioplasty material of choice in children are non-resorbable hydroxyapatite cements.
3) Hydroxyapatite cements are the most biocompatible cranioplasty material and will grow with the skull bone as it expands outward.
Dr. Barry Eppley
Indianapolis, Indiana



