Introduction
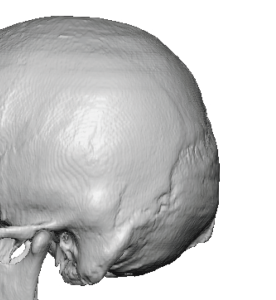
A back-of-the-head skull implant, also known as an occipital implant, is a cosmetic or reconstructive procedure designed to improve posterior skull projection, roundness, and symmetry. Common indications include:
- A flat or under-projected occiput (most often congenital)
- Imbalance in head shape where the front or sides are well developed but the back appears flat
- Asymmetry resulting from birth conditions, trauma, or prior surgery
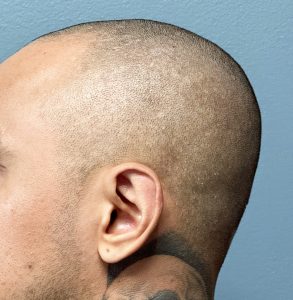
Most patients with a flat back of the head desire a stronger, rounder contour, which is particularly noticeable in profile and posterior views. Men present more frequently than women for occipital augmentation, likely due to shorter hairstyles and reduced hair coverage that make posterior skull deficiencies more visible
Implant Design and Material Considerations
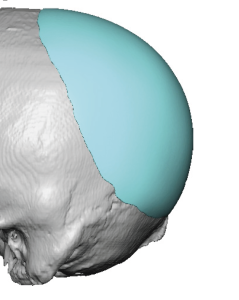
Back-of-the-head onlay augmentation is best performed using a custom-designed skull implant based on the patient’s 3D CT scan. These implants are fabricated from solid medical-grade silicone and are designed to precisely match the patient’s skull anatomy. This approach provides the most natural shape, optimal symmetry, and predictable projection.
The primary alternative material is PMMA bone cement, which offers more limited projection capabilities and is associated with a higher risk of surface irregularities and edge visibility. For these reasons, custom silicone implants are the preferred option for occipital augmentations of any significance.
One important anatomic feature of the back of the head that is often not appreciated and affects the implant design is that the lower end of the visible occipital bone does not go as low on the back of the head as many think. The lower end of the bone sits roughly at the level of the external ear or just below that of the brow bones on the forehead.
Custom occipital implants provide permanent improvement in posterior skull contour and overall head balance. Typical recovery includes:
- Swelling: Peaks within the first 48 hours
- Soreness or tightness: Common for 1–2 weeks
- Return to work: 7–14 days for non-physical occupations
- Final shape: Apparent by approximately 6–8 weeks
Case Study

Discussion: Determining Implant Projection
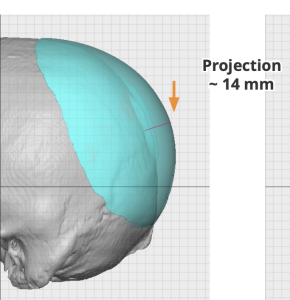
When designing custom skull implants, two primary factors must be considered:
- Implant footprint (the surface area of skull coverage)
- Implant projection (the degree of posterior augmentation desired and tolerated)
Implant Projection Ranges
Modest Projection (6–10 mm)
- Subtle but clearly noticeable enhancement
- Very natural appearance
- Lowest risk of scalp tightness or healing complications
Moderate Projection (10–15 mm) (most common range)
- Produces a stronger, rounder occiput
- Still appears natural in most patients
- Requires adequate scalp elasticity
Large Projection (15–20 mm)
- Creates a dramatic change
- Appropriate only when:
- Scalp elasticity is sufficient, or
- The patient has had a prior implant
- May require staged scalp expansion to reduce the risk of tightness, pressure, shock hair loss, or wound-healing issues
Factors Influencing Safe Projection
1. Scalp Elasticity (Most Critical Factor)
Scalp thickness and elasticity determine how much implant volume can be safely accommodated. Thicker scalps—often associated with increased pigmentation and darker hair—generally have greater elasticity. Excessive projection relative to scalp thickness can lead to pressure pain, shock hair loss, or incision healing problems.
2. Skull Shape
A very flat occiput typically has tighter scalp coverage and may tolerate less projection. Conversely, skulls with some existing curvature may safely accept greater implant volume.
3. Width-to-Projection Balance
A narrower skull may appear fuller with less projection. Effective implant design often reduces the need for extreme posterior projection by increasing width and contour blending.
4. Hair Thickness
Thick hair visually amplifies projection and contour changes. Thin hair may indicate a thinner scalp with reduced elasticity and less tolerance for large implants.
Gender Differences in Occipital Aesthetic Goals
Male Aesthetic Goals
- Transition from flat to gently rounded (not bulbous)
- Broader posterior contour
- Smooth blending into the parietal regions
- Design emphasis:
- Width over height
- Lower-to-mid occipital fullness
- Balanced profile with forehead and jaw
Female Aesthetic Goals
- More rounded and vertically curved occiput
- Smooth, continuous skull arc
- Narrower, tapered implant edges
- Design emphasis:
- Shape over size
- Higher occipital curvature
Based on experience, men generally tolerate—and often require—more projection than women, though typically less than they initially expect. The most consistently ideal outcomes fall within the single-digit to low-teens millimeter projection range.
Key Points
- Back-of-the-head augmentation is most effectively performed using a custom-designed skull implant that optimizes both projection and shape.
- Achievable implant projection represents a balance between the patient’s aesthetic goals and the scalp’s ability to stretch and safely accommodate implant volume.
Barry Eppley, MD, DMD
World-Renowned Plastic Surgeon
Sources