Introduction
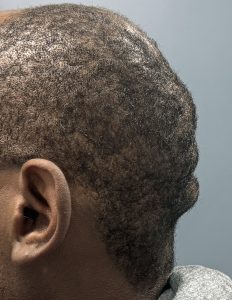
An occipital bun is a rounded overgrowth of the occipital bone at the back of the skull. This produces an exaggerated posterior curvature that disrupts the normal, smooth convex contour of the back of the head when viewed in profile. It represents a normal anatomic variant of skull development rather than a true bony pathology. Most occipital buns are asymptomatic, but in some individuals they are cosmetically bothersome or cause discomfort and pressure when wearing helmets or hats.
Surgical management is purely aesthetic and consists of an open occipital osteoplasty (direct bone reduction). Through a posterior scalp incision—typically transverse or gently curvilinear and placed within the hair-bearing scalp—the occipital bone is exposed in a subperiosteal plane. A high-speed burr is then used to reduce and smooth the bony prominence. The goal is not to create a flat posterior skull, but rather a reduced, natural-appearing convex contour.
Bone Thickness Considerations
The most critical factor in occipital bun reduction is the thickness of the occipital bone. This determines not only the safety of the procedure—by avoiding excessive thinning, dural exposure, or intracranial violation—but also whether enough bone can be removed to produce a meaningful cosmetic improvement. Establishing safe depth limits for bone reduction is therefore essential.
Average occipital bone thickness ranges from 12 to 18 mm, though it may be as thin as 8 to 10 mm in some patients. The thickest portion is typically central and inferior, with thickness decreasing laterally. Bone thickness should never be assumed, as there is wide interpatient variability. In the author’s experience, greater skin pigmentation often correlates with increased skull bone thickness, although this observation is not absolute.
General guidelines for safe occipital bone reduction include:
- Maximum reduction: up to 50% of the measured bone thickness
- Absolute maximum in cosmetic cases: approximately 5–7 mm, and only when CT imaging confirms adequate bone thickness
- Target endpoint: preservation of at least 5 mm of residual bone over the dura
Ideally, a preoperative 3D CT scan should be obtained, with color mapping of skull thickness over the planned area of reduction. When occipital bone thickness exceeds 10 mm, adequate and aesthetically effective reductions can usually be achieved.
Intraoperatively, safe depth can also be assessed by observing the transition from dense cortical bone to the more vascular diploic space, which signals proximity to depth limits.
Bottom Line
Occipital bun reduction can be highly effective, but the degree of correction is governed by how much bone can be safely removed. Because the occipital bone is the thickest bone of the skull—and the occipital bun represents an overgrowth of this thick bone—adequate reduction is possible in the vast majority of patients.
Case Study




Discussion
Although many occipital buns are not associated with scalp rolls, a subset of patients—particularly those with thicker or more lax scalps—exhibit horizontal folds or ridges of scalp tissue. These rolls may result from inherent scalp laxity, posture-related folding during neck flexion, or bunching of loose scalp tissue against a prominent occipital bone. Short hair or shaved scalps make these folds more conspicuous.
Scalp rolls may present as a single fold or at multiple levels, sometimes numbering as many as three. Importantly, reduction of the occipital bone alone will not improve these scalp rolls and may actually accentuate them. Partial or complete excision of one or more scalp rolls is often required to tighten the scalp and achieve a smooth contour over the reduced bone.
Key Points
- Occipital bun deformities may be associated with horizontal scalp rolls, depending on scalp thickness and laxity.
- Bone reduction alone will not correct scalp rolls; concomitant scalp roll excision is necessary.
- The scalp excision scar is only modestly longer than that used for standard bun reduction and typically heals just as well.
Barry Eppley, MD, DMD
World-Renowned Plastic Surgeon