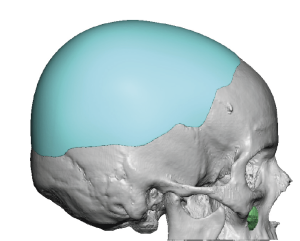
Background: Skull implant augmentation is unique in many ways that largely revolve around its overlying scalp coverage. Besides its visibility the most important feature of the scalp is its tight adherence to the skull. It is best thought of as skin stretched over a beach ball. The point being is that it is tight and this tightness has a major impact on any skull augmentation procedure. It will affect how much skull augmentation can be achieved.
The scalp does have some flexibility when detached from the bone which is influenced by its thickness. Thicker scalps are more elastic than thinner scalps. The thickness of the scalp is directly related to the patient’s ethnicity and skin pigmentation. The lighter the skin pigment and hair color the thinner the scalp usually is. Conversely the darker the skin pigment the thicker the scalp is. The thicker the scalp is the more flexibility it has and the greater skull augmentation effect that can be achieved by an implant pushing outward under it.
Another important variable that can affect scalp flexibility in potential skull augmentation patients is a history of hair transplantation. If a strip hair harvest has been previously done scalp flexibility will be decreased due to the lost scalp tissue. Any other excisional procedures (e.g., frontal hairline advancement) creates the same loss of scalp flexibility.
Assessing scalp flexibility in any skull implant procedure is important but is paramount in larger augmentation needs when the scalp flexibility is limited. This problem is circumvented by the use of a 1st stage scalp expander. After its placement it is slowly inflated by the patient to reach a fluid volume that is equivalent to the volume of the designed skull implant. This is usually a process that takes up to 3 months to achieve sufficient scalp expansion.




Case Highlights:
1) Most females with small heads that want a significant skull augmentation require a 1st stage scalp expansion.
2) Any patient for skull augmentation that has had a hair transplant strip harvest scar will need a 1st stage scalp expander.
3) The scalp expander can be placed through the hair transplant harvest scar with little liquid fill at the time of placement.
Dr. Barry Eppley
World-Renowned Plastic Surgeon






