Background: Of all the standard facial implants that are available none is harder to properly position than the jaw angle implant. This is due to three reasons; 1) the working end of the jaw angle implant can not be seen from the intraoral incision, 2) the implant placement is in the most posterior part of the jaw where adequate subperiosteal pocket dissection requires a good understanding of the bony and muscular anatomy of the jaw angles and 3) it is a paired aesthetic structure which induces its own risks of asymmetric implant placement. As a result it is not quite as simple as making a pocket and simply sliding an implant into it.
Having performed other types of jaw angle surgeries such as sagittal split osteotomies and jaw angle fracture repairs is helpful, and actually technically more challenging, they differ in ways that are uniquely different from jaw angle implant placement. The sagittal split osteotomy is performed at the front region of the jaw angles where the bone cuts are largely performed under direct vision. Jaw angle fractures are often done through skin incisional approaches where the fracture alignment is clearly seen. And even if done intraorally the complete fracture line does not need to fully visualized to achieve a good repair.
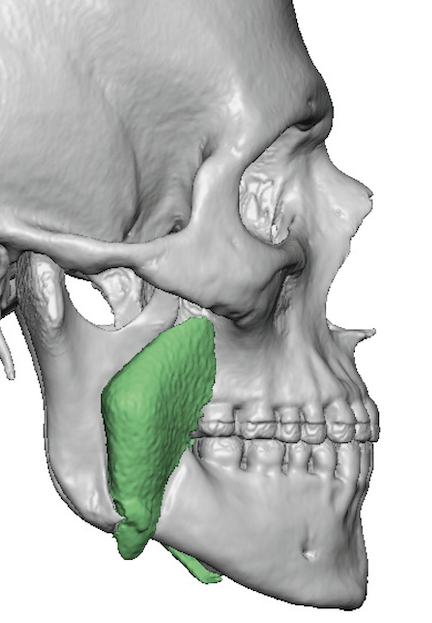
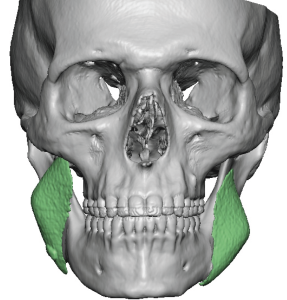
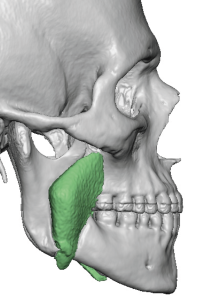
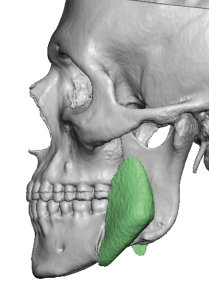
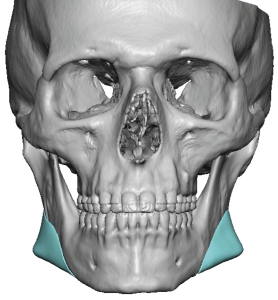
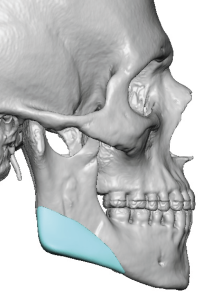
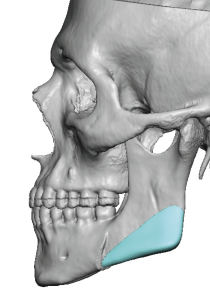
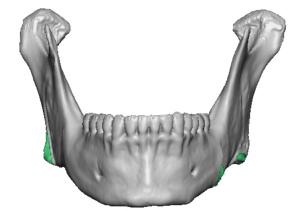
Whether highly experienced or not the most common reason for jaw angle placement is inadequate posterior pocket development. The most common reason is that the ligamentous attachments and the posterior muscle border is not elevated resulting in an anterior location of the implant. This pushed the widening implant too far forward not putting the angle augmentation in the right location. With a vertically lengthening implant an undesired widening effect is created with no vertical increase at all.
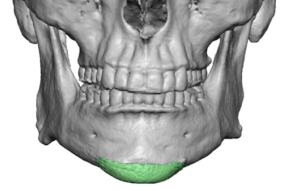
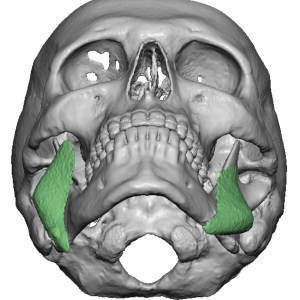
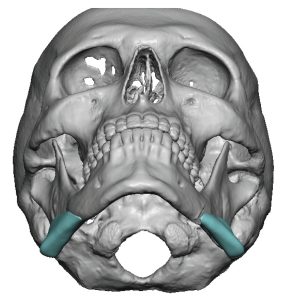


This is a fairly severe case of jaw angle implant malpositioning that was so significant one wonders if they had ever done the procedure before. At the least the extent of intraoral dissection was woefully inadequate and it is clear that they did not appreciate where the posterior border of the ramus was located. They got fooled by not knowing that the bony jaw angle turns inward behind the last molar tooth which makes the posterior border very hard to see.
Key Points:
1) Jaw angle implant malpositions take on predictable patterns due a lack of anatomic understanding and inadequate pocket development as a result.
2) Intraoral visualization is inadequate to ensure that the jaw angle implant is in proper position over the genial angle.
3) Custom jaw angle implants may provide shape improvements over standard implants but they still have to be properly placed to get the full benefits of the design.
Dr. Barry Eppley
World-Renowned Plastic Surgeon