Background: Testicular enhancement is a conceptually different procedure from testicular replacement. Replacement is a reconstructive procedure to implant a substitute for what has been lost. Enhancement is to enlarge the appearance of testicles that are intact…small but present. Both younger and older men present for testicular enhancement but often for slightly different reasons. The older male has lost testicle size due aging and hormone replacement.
For testicular enhancement implants can be used two different ways…displacement and wraparound. Displacement is a simpler implant concept that can be effective when the desired implant size is significantly greater than that of the natural testicle. (50% to 100% bigger) The larger implant pushes aside the smaller testicle and becomes the dominant structure in the scrotum. Conversely the wrap around technique makes an implant in which the smaller testicle fits inside it with a small opening on one end for the cord. While this can be used for any implant-testicle size discrepancy it theoretically is most indicated when the desired enhancement is more modest.
While the wraparound testicle implant concept has tremendous appeal it also has the higher complication risk. Separation of the testicle out of the implant (extrusion) can occur since the testicle has an attached cord that can retract and the implant does not fuse directly with the wall of the implant. While this occurrence is not common it is also not rare. How to assuredly prevent that postoperative risk has not yet been solved.
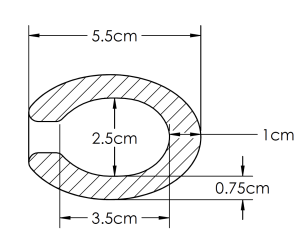


The relevant long term question is whether a more precise fit of the natural testicle inside the implant based on ultrasound measurements will help lower the risk of potential postoperative testicle-implant separation. That is a question only time will answer. But moving forward I think this is the best way to do the wrap around testicle implant enhancement concept.
Highlights:
- In very small testicles in younger men the wraparound implant for testicular enhancement has great appeal.
- The main problem with wraparound testicle implants is the risk of postoperative extrusion or separation of the testicle out of the implant.
- Matching the actual size of the patient’s testicles to the design of the inner chamber of the hollow testicle implant may lower the risk of postoperative extrusion.
Dr. Barry Eppley
World-Renowned Plastic Surgeon







