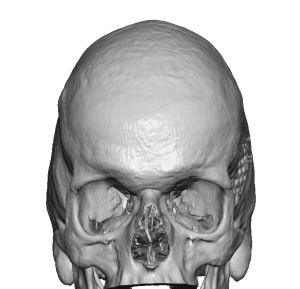
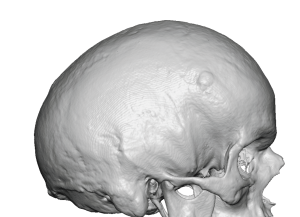
Background: Scaphocephaly is a general term that literally means a boat-shaped head. Dimensionally this means an elongated front to back head length that is invariably associated with a narrow head width as well. This can occur in non-syndromic patients but the expression of the altered head shape is more mild in presentation than in syndromic cases. Syndromic scaphocephaly always refers to congenital sagittal craniosynostosis which creates a more severe head shape abnormality and is most commonly treated by early cranial vault remodeling surgery.
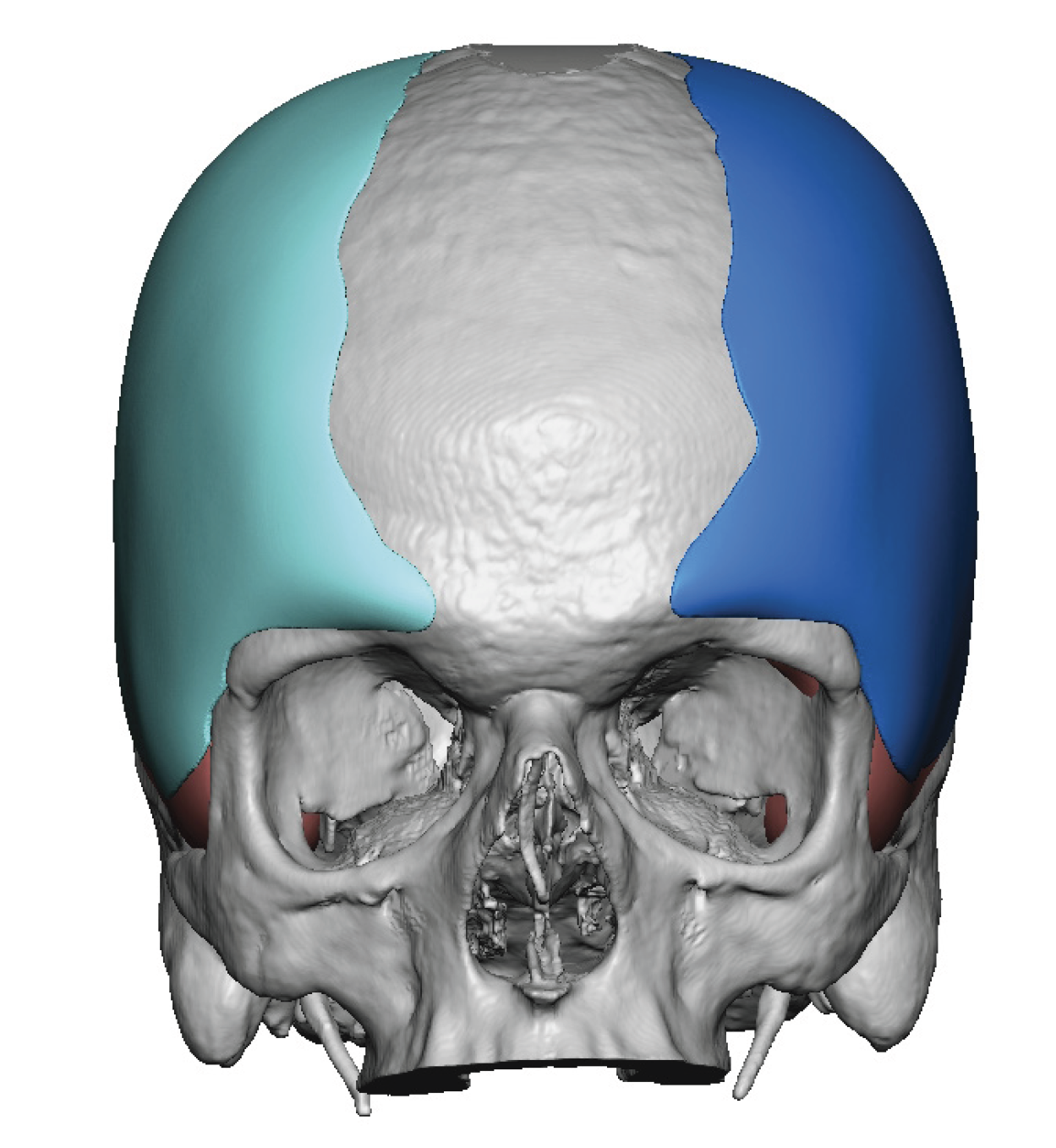
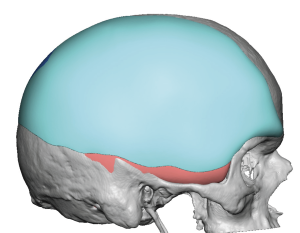
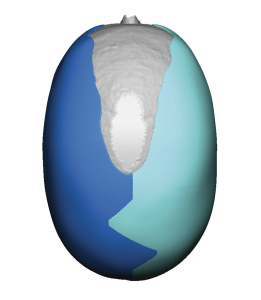
But untreated sagittal craniosynostosis patients still do occasionally occur and present for head reshaping. Unlike infants and very young children the use of cranial vault reshaping techniques in adults is not going to be effective’s or even practical, given the thickness of adult skull bone and is limited ability to heal gaps in the bone. In adults the narrow skull shape must be treated by augmentation on top of the bone and muscle…in which a good deal of width can be added. The elongation of the skull is still treated by autologous bone manipulations which for reduction involves bone burring. Such front to back reductions are more limited than the head widening that can be achieved. But each dimensional change is synergetic no matter what the magnitude of its effects are.
One of the common misconceptions about alloplastic head widening is that the implant must be placed beneath the muscle on the side of the head. While it is always good to have an implant placed as deep in the tissues as possible to reduce the risk of complications (infection, seroma, implant edging) this doesn’t work forehead widening as the muscle will retract, the amount of implant show will be limited and the augmentation can not cross the bony temporal lines in either the forehead or onto the back of the head. In significant head widening, which is certainly what an adult scaphocephalic head shape needs, it is necessary to cross the bony temporal lines. To do so this requires being on top of the temporal muscle/deep fascia.


He went on to fully heal without infection or any problems with incisional healing. He did develop seromas after his drains were removed which requires secondary drain placement to fully resolve.


Key Points:
1) Congenital scaphocephaly in an adult is primarily treated by a custom skull implant with the objective of head widening.
2) The head widening implant can be combined with some limited reduction of the anteroposterior length of the skull.
3) A existing coronal scalp scar provides the ideal access for surgical placement of a large head widening implant.
Dr. Barry Eppley
World-Renowned Plastic Surgeon