Background: The concept of skull reduction is like the reduction of almost any skeletal structure in the body…there are limits. The length and thickness of the anatomy is one controlling factor along with how well the overlying soft tissues shrink and contract down around the reduced bone. Thus most aesthetic reductions have to be given good thought beforehand to whether the surgery can create enough of a result to justify the effort.
The limiting factors for skull reductions are the thickness of the bone and/or temporal muscle and the scalp’s ability to shrink down to show it. But when patients think/inquire about skull reduction they may be asking about two fundamentally different objectives. One type is spot or limited skull reductions. This means that one, two or three surfaces of the skull are being treated with the objective of reducing their prominences. This is usually successful in most of the cases despite the anatomic limitations. The other type of skull reduction is when patients ask about making their overall head smaller…in other words treating all five surfaces. This type of skull reduction may be less successful as the anatomic limitations of five surfaces added together may not produce enough circumferential reductive change.
One spot area of skull reduction is at the top of the head. When it comes to top of head reduction patients may have two related bit different objectives. One objective is to the height of the convexity which usually refers to an elevated curve seen in profile from the coronal suture lines back to the crown area. The other objective is a more exaggerated form of top of head reduction in an effort to visible reduce one’s height. The former is successful, the latter is not. Flattening a convexity does not make a substantial height reduction.
Case Study: This male had a life long Conner about the height in the top of his head. He sustained head trauma as a child on the top of his head and he felt this was the nidus for its overgrowth as well as the source for being teased for having a big head. His lateral skull x-ray showed that enough outer cortex existed to make the procedure worthwhile.

Drains were used for 24 hours after the surgery and he went not to heal uneventfully. Four months later he came back to have more bone removed from the back of the crown that could not be reached from the initial scalp incision. A small secondary scalp incision was made way behind the first one and the surgery was done in the prone position.

In hindsight it all could have been done through a single long coronal scalp incision from ear to ear in a single surgery. But this is the challenge in skull reduction surgery…how much incisional length can be tolerated. In more limited scalp incisions, which are commonly used, as much bone surface areas is treated as can be reached…with the hope that it is enough.
Key Points:
1) The limits of skull reduction are the thickness of the outer cortex of the skull and the incision permitted to do it.
2) It is usually best too think of skull reduction as affecting specific area of the head rather than making the overall head smaller
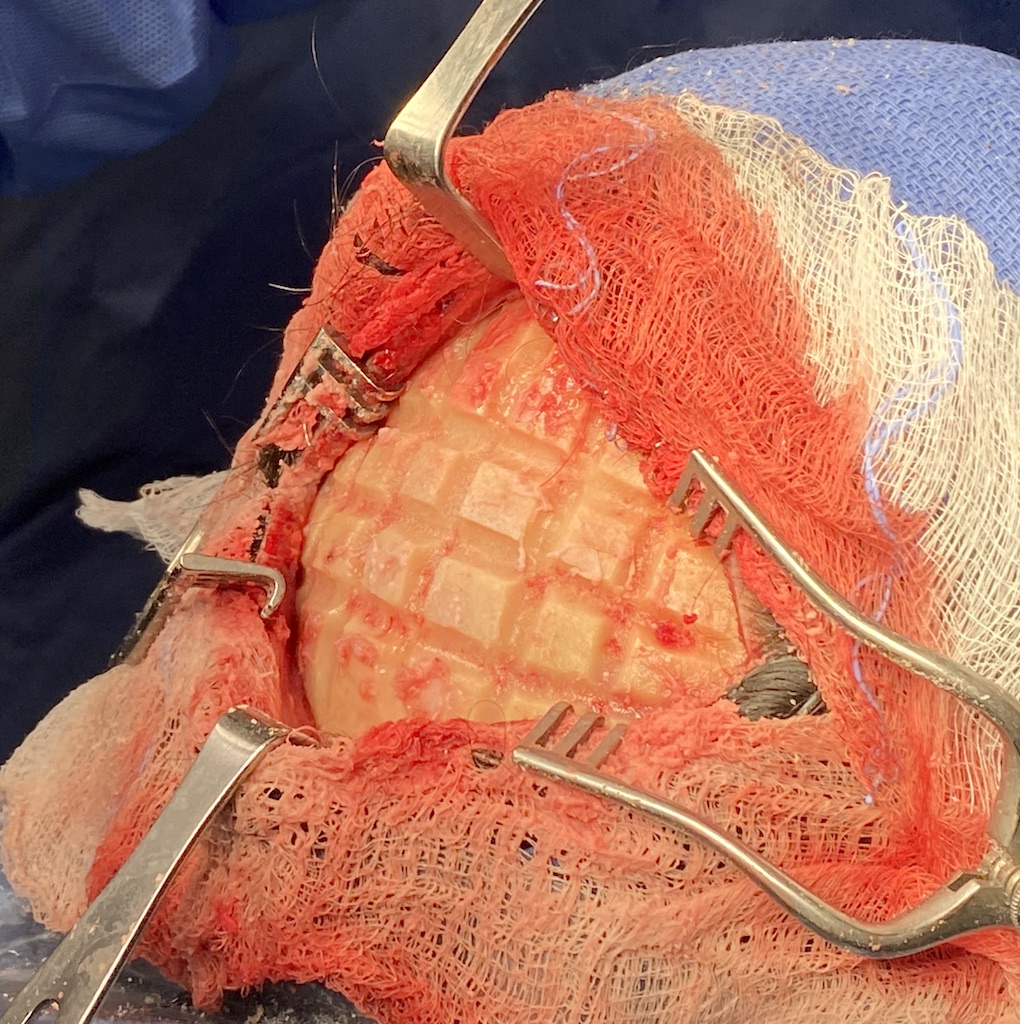
3) Larger surface area skull reductions require a systematic grid approach for maximal effectiveness.
Dr. Barry Eppley
World-Renowned Plastic Surgeon