Surgical treatment of the downturned corner of the mouth has historically been associated with two common themes. First it is a procedure by history that has been largely done in age-related drooping mouth corners. (older patients) Two, it is a laterally-based procedure that lives visible scars with a high rate of adverse scarring. Both trends as mentioned are historic as younger patients today are interested in improving their static mouth posture and newer techniques have improved their aesthetic outcomes.
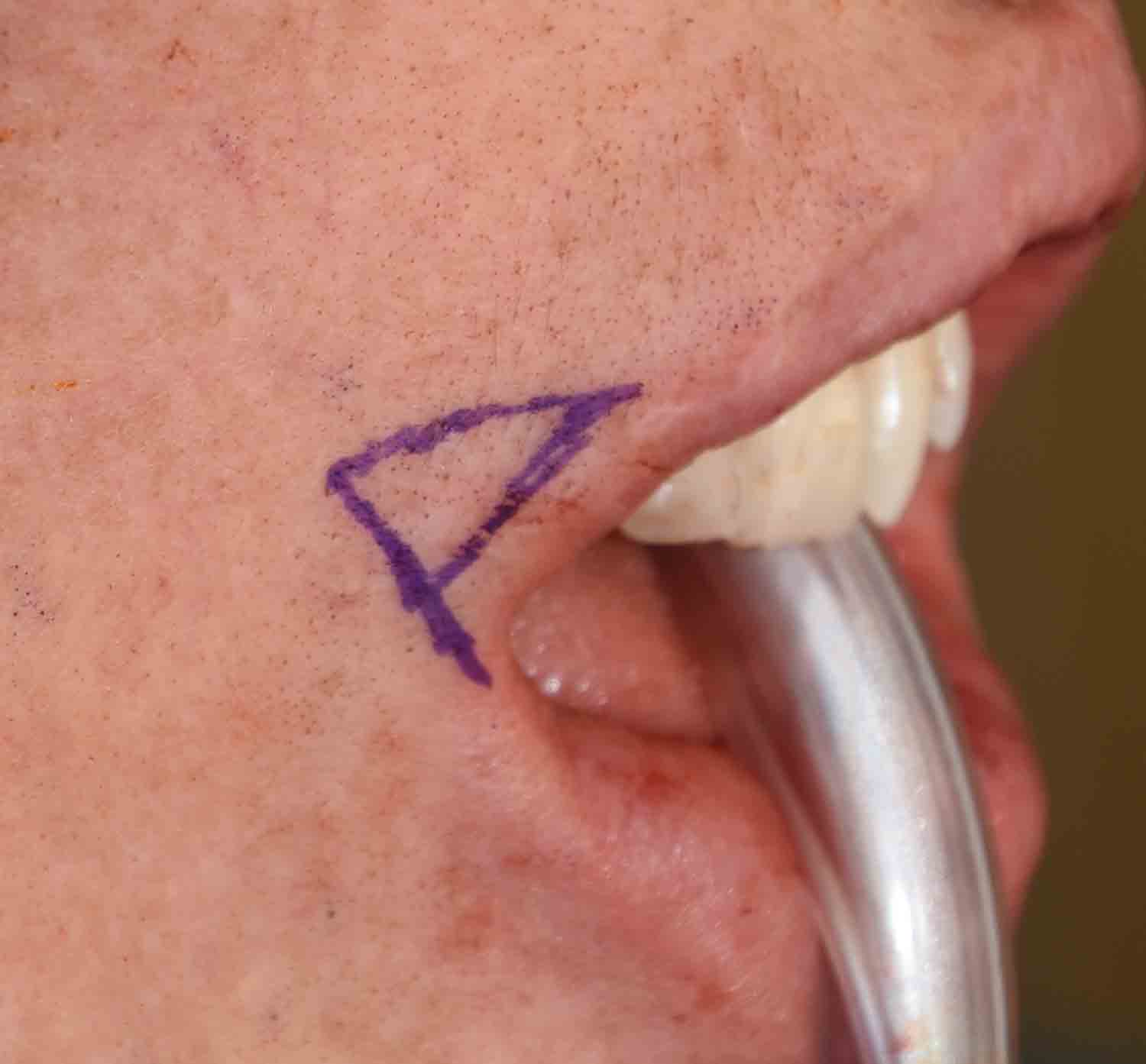
In the November 2020 issue of the journal Archives of Plastic Surgery an article was published entitled ‘A Modified Method for Corner Mouth Lift in Scar-Prone Patients’. In this paper the authors describe a corner of the mouth lift technique which includes a triangular skin excision and transposition of a vermilion flap after release the orbicularis muscle to relieve the tension. Over a nearly three year period a total of three hundred twelve (312) patients were treated with this corner mouth lift technique. The overwhelming number were young females (greater than 90%) with a mean age of 30 years old. About a third of the patients had the corner mouth lift only while two-thirds had other perioral procedures.

What was not reported in this paper, and is of particular importance, is what the rate of scar revision was in this large number of patients. What I know is that with 624 corner mouth scars, the scar revision rate is not zero. I would have loved to know what the number of scar revisions that were needed in this young patient population. Suffice it to say that every patient considering this procedure needs to know that this risk exists and I wouldn’t consider it a small one. This does not mean the procedure is not worthwhile but every corner of mouth lift patient needs to factor this potential secondary need into undergoing the primary corner mouth lift procedure.
Dr. Barry Eppley
Indianapolis, Indiana