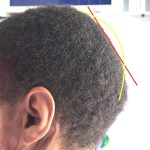
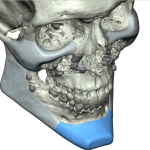
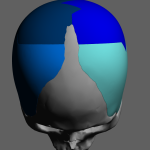
Plastic Surge Case Study – Combined Bony and Soft Tissue Occipital Knob Reduction

Background: The occipital knob is a natural spike of bone on the visible end of the bony back of the head. Why it gets more visible in some people is not known although it appears to be more gender specific as I have seen it in many men but never yet in a woman. This Read More…