Plastic Surgery Case Study – Secondary Custom Infraorbital-Malar Implants after Bimaxillary Advancement Surgery
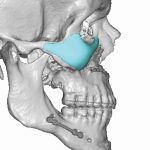
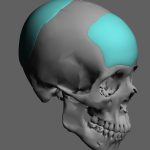
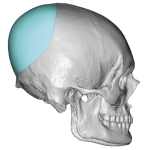
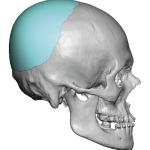
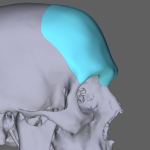
Background: Bimaxillary or double jaw advancement surgery is a very effective procedure for obstructive sleep apnea in properly selected patients. By moving the maxillomandibular bony complex forward by a significant amount, usually 8 to 10mms, the nasal and oropharyngeal airway space is opened up for improved air flow. While functionally effective the tradeoff for such Read More…