Background: The skull, while often perceived as a solid piece of bone, is not. It is actually composed of three layers, very much like an Oreo cookie. There are the outer and inner solid cortical layers (the cookie) and then there is a thinner inner layer which is softer known as the diploid or marrow space. (the filling)
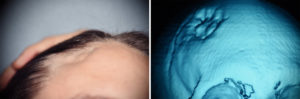
Many skull defects occur as a result of injuries caused by fractures of varying degrees of the bone’s thickness. When the skull fracture does not significantly displace the inner cortical table and does not disrupt the dura, there is no need for surgical reduction. But such fractures often do displace the outer cortical table resulting in contour defects. The soft tissue will eventually follow the depressed bone inward as scar contracture and healing ensure.
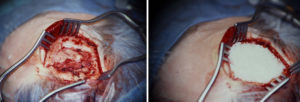

The use of hydroxyapatite bone substitute today in skull reconstruction, and for almost the past twenty years now, has been with using it in a bone cement form. This provides the best method of application as it is contoured into the defect site and then sets before wound closure. But hydroxyapatite can be still used in granular form which allows for true fibrovascular ingrowth and even some bone ingrowth as well. Its use is restricted to a completely contained skull defect with an underlying floor and walls.
Highlights:
- Small skull defects can be treated by a wide variety of cranioplasty materials.
- In a small partial-thickness skull defect, hydroxyapatite granules can be used to fill the defect and create a smooth cranial contour.
- A resorbable cover can be used as a roof for a hydroxyapatite granule skull reconstruction.
Dr. Barry Eppley
Indianapolis, Indiana



