Background: Since chin reduction is not as commonly requested or performed as chin augmentation the techniques to do so are not often well understood. In the traditional macrogenia female, the reflex operation for most plastic surgeons is an intraoral burring chin reduction technique. It is a reflex operation because the first thought is in how to do it in a scarless manner. While the intraoral approach is scarless and decent results are possible in the properly selected patient, it is a dimensionally limited procedure with a potential for soft tissue issues.
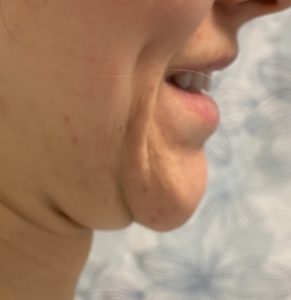
To do an intraoral approach the soft tissue chin pad must be detached from the bone through subperiosteal elevation. This permits the bone to be reduced in the horizontal and width dimensions. (but not vertically) With the closure of the intraoral incision what is not apparent is there is now a loss of bone support and a relative excess of the soft tissue chin pad. While some soft tissue contraction of the chin pad can occur, like in all soft tissues, the chin pad is unique because it is stretched out tissue over a projection point. Thus when it contracts it tends to ball up rather than lay completely flat/smooth. This can result in a chin pad ptosis with fullness off the end of the chin bone that is magnified when one smiles.
Correcting soft tissue chin pad excess/ptosis is not usually effective done by intraoral resuspension. It may help somewhat by you can’t lift away or resuspend soft tissue excess. Again the intraoral approach is appealing but that should not be confused with effectiveness.



Case Highlights:
1) An intraoral chin reduction can result in soft tissue chin pad ptosis due to loss of bone support and periosteal attachments
2) Attempts at intraoral chin pad resuspension frequently fail as a major component of the problem is a now excessive soft tissue chin pad where some reduction is needed.
3) The submental approach allows for a combination of redundant tissue excision and chin pad tissue tightening.
Dr. Barry Eppley
Indianapolis, Indiana






