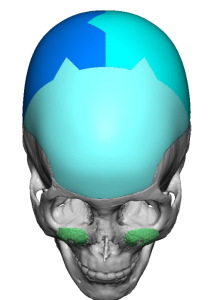
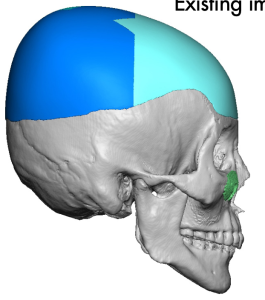
Background: Aesthetic skull augmentations, like any other face and body areas, requires the placement of an implant to create the desired effect. What differentiates such skull augmentations is there are no preformed off-the-shelf implants to do so and the overlying soft tissues (scalp) imposes some natural implant size limitations due to its natural tightness. The first requirement is currently overcome by a preoperative implant design process. Adequate scalp laxity to accommodate the implant, if needed, can be created by a scalp expander prior to implant placement.
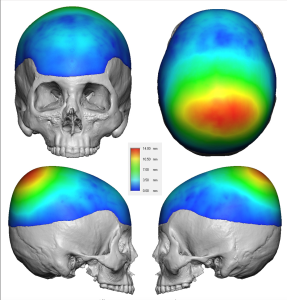
There is no accurate method to know precisely whether one’s scalp can stretch enough to allow a skull implant of some size to be placed underneath it. Scalp stretch with undermining varies amongst patients based on their scalp thickness. Skull implants also cover a large surface area in which its volume can add up quickly and the implant’s thickness at its maximal area of projection belies its volumetric impact. It is also important to recognize that the desired use of a small scalp incision does not create the same implant space that a large bicoronal scalp incision with undermining does. (but no patient wants that incision for an aesthetic procedure)
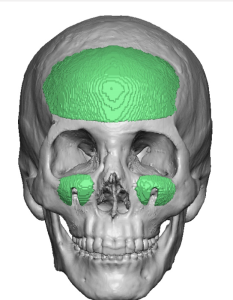
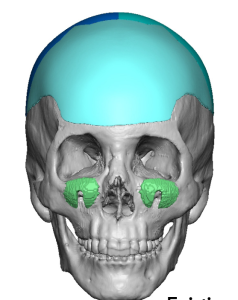
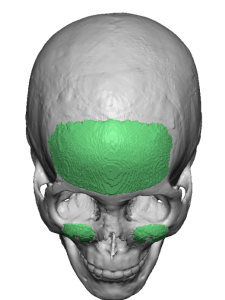
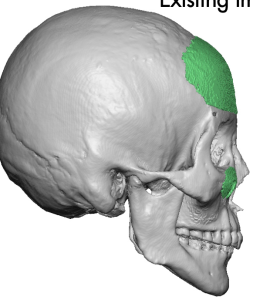
Despite the lack of a known preoperative method to determine whether a skull implant will fit there are some general guidelines. Skull implant volumes of 150ccs are about the maximum for most patients. Thin scalps in females will be less, thicker scalps can be a bit more. A history of hair transplants, particularly with a strip harvest, is usually a strong indicator of limited scalp flexibility. Implant designs that cover more than 1/2 of the skull’s surface or have maximum projections greater than 12 to 14mms at the limits of most scalp’s ability to safely cover over it.
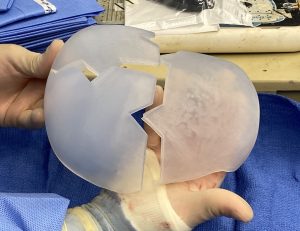
Thus in large skull implants the limitations of the scalp can be overcome by a first stage scalp expander. Getting a large skull implant through a smaller non-bicoronal scalp incision requires a multi-piece skull implant design.





Key Points:
1) The need for a two stage approach to large aesthetic skull augmentations depends on the volume of the designed implant and how much the scalp can stretch to accommodate it.
2) The amount of scalp expansion needed is volumetrically similar to that of the designedskull implant to be subsequently placed.
3) To keep scalp incisions small the skull implant is designed in multiple pieces to be fully assembled once inside the subperiosteal pocket.
Dr. Barry Eppley
World-Renowned Plastic Surgeon