Technical Strategies – Subfascial Fat Injections for Temporal Augmentation in Custom Forehead Implants
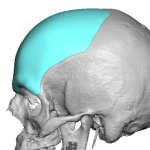
Augmentation of the upper third of the face is ideally done with a custom forehead implant design. In creating these designs one of its considerations is whether the augmentation should stop at the bony temporal line or does it need to extend onto the temporal muscle area at the side of the forehead. As a Read More…









