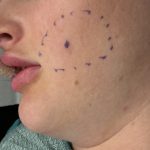
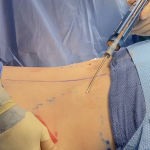
Plastic Surgery Case Study – Webbed Neck Correction Combined with Otoplasties and Submental Liposuction

Background: The webbed neck is a well known congenital deformity that is associated with many different syndromes and conditions, most notably Turner’s syndrome. Its embryology is not precisely known although it is somewhat simplistically obvious looking at facial development and the migration of the ears upward from the neck at around 7 to 8 weeks Read More…