Combination Browlift and Frontal Migraine Surgery

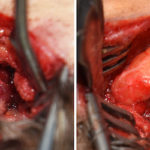
One of the essential steps in any form of a browlift is a periosteal release along the superior orbital rims. In so doing it is necessary to locate and release the tight tissues around the supraorbital nerves. Its purpose is to protect the nerves in the processing of ensuring the lower forehead tissues are adequately Read More…