Plastic Surgery Case Study – Reduction of the Male Single Occipital Scalp Roll

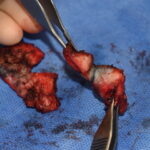
Background: The scalp is pierced as a homogenous layer of soft tissue covering the skull whose most dominant feature is the hair it may or may not contain. While the scalp does have five distinct layers throughout its large surface area of coverage the thicknesses of it varies. The thickest part of the scalp is Read More…