Plastic Surgery Case Study – Head Width Reduction with Temporal Bone and Muscle Removals
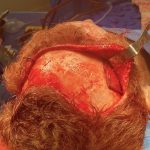
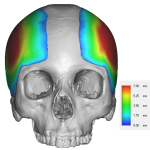
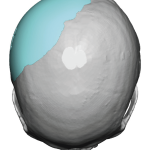
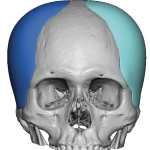
Background: The wide or light bulb shaped head is caused by a combination of excessive bone and soft tissue. The temporal muscle makes up a significant part of the width of the head particularly at the anterior temporal area. (temporal fossa) It is disproportionately wide compared to the cheek and jaw bony widths below it. Read More…