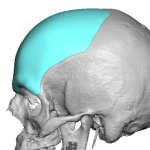
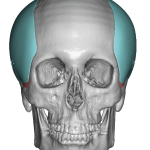
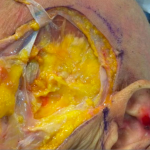
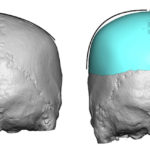
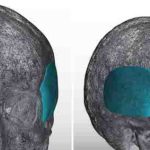
Plastic Surgery Case Study – Type 4 Temporal Augmentation Wrap Around Head Widening Implants
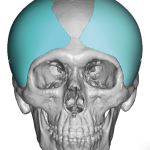
Background: All areas of the skull can be aesthetically augmented with custom designed implants…the most effective method to do so. Augmenting the side of the head is unique, however, because most of it is covered by muscle and not bone. The most important landmark for the side of the head augmentation is the bony temporal Read More…