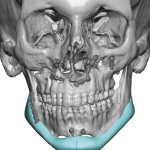
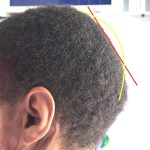
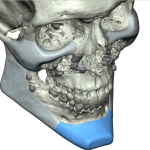
Plastic Surgery Case Study: Submental Replacement of an Oversized Su-Por Chin Implant in a Female
Background: Aesthetic facial implants are currently available in numerous different materials with a wide variety of sizes and shapes. While each manufacturer of the different materials tout their benefits the reality is that there is no perfect implant material that has all of the benefits both surgeons and patients desire. Each material has its advantages Read More…