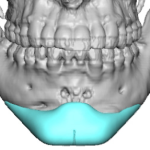
Technical Strategies – Mesh Implant for Small Surface Area Minimal Thickness Skull Contour Defect

Aesthetic skull augmentations today are most effectively done by a custom skull implant design. Gone are the days of the use of PMMA bone cements, which may be fine as an inlay method for skull bone defects which is their history. But PMMA bone cements is not a highly effective method as an onlay contouring Read More…